Emergency discomfort is not clean. It shows up in layers, formed by physiology, fear, context, and the clock. I have seen a tranquil young adult grit teeth via a broken span, and an older male spiral from an easy hip crack into ecstasy due to the fact that his discomfort was undervalued and undertreated. PUAEME008, the nationwide unit typically referred to as Provide Discomfort Management, exists to close that void in between theory and the bedside. When shown and applied well, it gears up clinicians and -responders to bring alleviation quickly, safely, and consistently.
This is not just about pressing analgesics. It is about organized assessment under stress, choosing the best modality for the client in front of you, and having the operational discipline to paper, turn over, and review. If you are taking a look at a pain management course, whether as component of prehospital training or a hospital-based upskill, recognizing just how PUAEME008 plays out in the field aids you select intelligently and exercise with confidence.
What PUAEME008 actually covers
On paper, PUAEME008 Offer Pain Management establishes efficiency requirements around assessing discomfort, carrying out accepted analgesia, keeping an eye on actions, and communicating efficiently with getting groups. In practice, the system is a scaffold for judgment. It requires you to integrate professional pattern acknowledgment with plan proficiency and human communication.
The core consists of: building a dependable pain history under time pressure; making use of verified devices such as mathematical rating ranges, Wong-Baker faces for children, and behavioral hints for individuals who can not self-report; preparing and supplying anesthetics within your scope; and observing, recording, and rising when the program differs plan. It is typically packed right into pain administration training programs for paramedics, occasion medics, first responders in remote industry, and some acute care registered nurses, although the details pharmacology and gadgets vary by jurisdiction.
I have actually seen 2 pupils with the same composed ratings do very in different ways when traveling. The one who excelled asked another question, checked another essential indication, and bargained with the individual as opposed to dealing with the chart. That is the distinction PUAEME008 intends to cultivate.
Pain evaluation when secs matter
An organized analysis does not suggest slow-moving. Succeeded, it ends up being a pattern you can run while relocating down a hallway or packing a client into an automobile. Start by securing the fundamentals: place, onset, character, intensity, radiation, organization with motion or breathing, and any type of warnings such as syncope, shortness of breath, or neurological deficits. A lot of clinicians stop after a solitary numeric rating. Numbers without context mislead. A "4 out of 10" from a stoic farmer with a flail chest does not amount to a "7 out of 10" from a youngster with a sprained ankle.
Observe for nonverbal cues. Guarding, pallor, diaphoresis, tachycardia, transformed respiratory system pattern, and frustration fill in voids when a client can not give information. For kids under seven or for nonverbal grownups, behavior ranges are frequently extra precise than attempting to compel a number. PUAEME008 stresses these options, and a good pain administration program will pierce them until they are second nature.
Reassessment is where several newbies slide. Pain hardly ever holds still. Activity, splinting, oxygen, or perhaps confidence can change it. Reconsider after interventions at intervals set by your protocol, usually every 5 to 10 mins at first, after that less often once stable. Record not only ball game, yet the individual's language. "Feels less sharp, more pressure." Those words matter, especially when handing over.

Pharmacology within range: alternatives and trade-offs
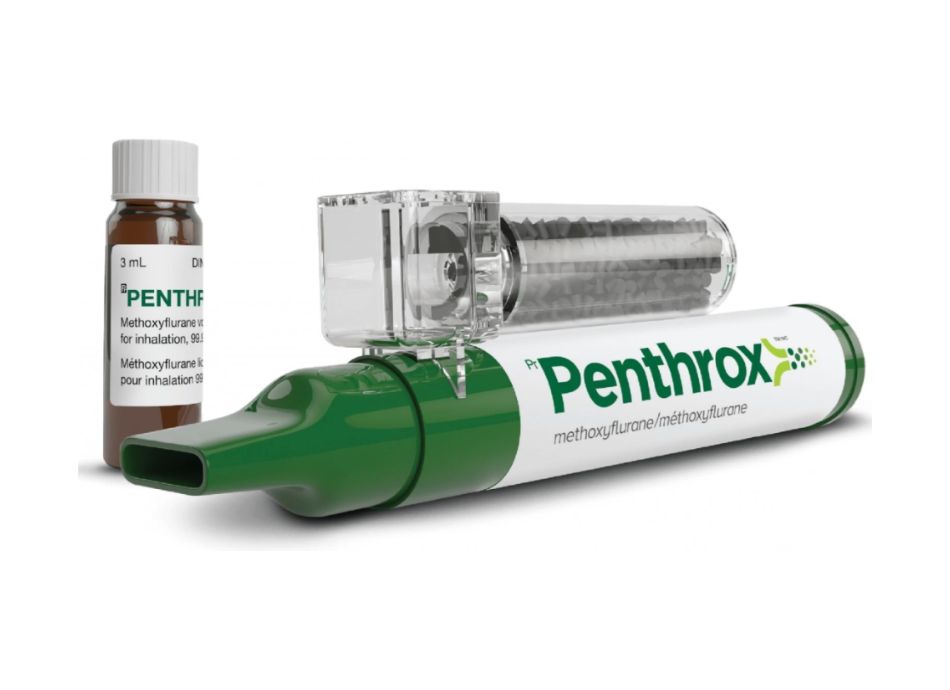
Protocols determine what you can give. Within PUAEME008 offer pain management frameworks, the usual suspects consist of breathed in methoxyflurane, fentanyl (intranasal or intravenous), morphine, ketamine in sub-dissociative doses, laughing gas 50-50 blends, and oral representatives where time and GI standing enable. Each has pleasant spots and pitfalls.
Methoxyflurane purchases time. It is rapid to provide, mobile, and well endured. I have actually utilized it on a hillside while waiting for a cot, its acquainted apple-pear smell a small convenience on a negative day. It is superb for modest stressful pain when IV gain access to is postponed or not required. It is much less excellent for individuals with considerable respiratory system compromise or prolonged management needs.
Intranasal fentanyl is a workhorse for fast analgesia without IV. It radiates in pediatric fractures and grown-up limb injuries, with a clean pharmacokinetic profile and very easy titration. Look for respiratory depression, particularly in older adults or when incorporated with sedatives. Clear interaction with your partner avoids piling doses also fast.
Morphine stays trusted for extreme discomfort, but it demands careful titration and surveillance for hypotension and oversedation. I save IV morphine for patients that need sustained alleviation and in settings where continual tracking is possible. It pairs well with antiemetics in patients susceptible to nausea.
Sub-dissociative ketamine has actually expanded in popularity since it protects respiratory tract reflexes while delivering solid analgesia and decreasing opioid needs. It can generate dysphoria or emergence phenomena, which are disturbing if you have not prepared the individual. A silent description and a calm tone lower that threat. Ketamine additionally aids in individuals with hypotension where opioids could get worse hemodynamics.
Nitrous oxide works and acquainted in some systems, less offered in others. It requires individual participation and is badly fit to those with breast injuries or believed pneumothorax. In the right situation, it supplies quick control with very little residual effects.
Nonpharmacological complements usually obtain buried under the enjoyment of medications, yet they pay returns. Splint well. Pad stress factors. Use ice bags judiciously. Change the atmosphere, dark extreme lights in migraine headache, limitation unneeded motion. A well-applied vacuum cleaner splint can decrease a pain rating by two points prior to any medication gets to the bloodstream.
Scope and policy: knowing the edges
PUAEME008 does not provide carte blanche. Your company's medical direction and neighborhood regulation identify which agents and courses are permitted. The best clinicians are those who understand their edge cases by heart. Typical plan supports consist of minimum age thresholds for methoxyflurane, cumulative dosage restrictions for fentanyl and morphine, contraindications for ketamine in specific psychoses or uncontrolled hypertension, and oxygen demands for laughing gas delivery.
When unsure, call early for clinical appointment if your system enables it. I as soon as handled a young adult with a femoral crack who had actually taken unidentified recreational compounds. The mix of energizer poisoning and trauma made opioid application treacherous. A fast seek advice from sustained a ketamine-first approach with conventional titration and constant monitoring. Profundity in these dilemmas comes from training and from confessing uncertainty when it matters.
Communication as an analgesic
Tone changes physiology. Dignity reduces supportive drive. Basic, straightforward sentences decrease concern. "You are risk-free. We are going to control your pain. You will certainly have the ability to breathe." I have actually seen discomfort scores drop a notch with those words alone.
Trust likewise safeguards against application mistakes. When an individual thinks you are paying attention, they share essential information: last dose of oxycodone, spots on their skin, a history of opioid-induced apnea, or inadequately regulated sleep apnea. For older grownups, validate drug listings and inquire about anticoagulants, as bleeding threat can reshape your functioning medical diagnosis and affect your choice of analgesic and transportation priority.
The handover seals care continuity. A beneficial handover tells a story: system of injury or beginning context, baseline discomfort description, adjustments after each treatment, complete dosages with timing, vitals patterns, and any kind of adverse effects. A hurried recitation of numbers without arc leaves the obtaining group rebuilding your reasoning. Strong PUAEME008 training demands that narrative clarity.
Special populations that check your craft
Pediatrics usually intimidates brand-new medical professionals. The antidote is prep work. Usage weight-based application graphes, keep intranasal devices within reach, and enlist caretakers to hold and relax. Youngsters mirror adult stress and anxiety. If you stay steady, they will typically resolve enough to accept splinting and intranasal analgesia without splits. Expect dehydration in extended abdominal pain, and prevent duplicating intrusive efforts that can wait for a regulated environment.
Older adults offer a various problem. Their pain resistance differs commonly, and their physiology conceals trouble. A small autumn with rib fractures can spiral right into hypoventilation and pneumonia if discomfort is undertreated. Equilibrium efficient analgesia with fall risk and ecstasy prevention. Low-dose titrated opioids or ketamine, hostile regional assistance where available, and early participation of obtaining groups make a difference.
Pregnancy changes whatever from gastric draining to respiratory reserve. Usage left lateral tilt when feasible, display fetal motions if progressed gestation, and select representatives with well-known safety and security accounts in your system. Nonpharmacologic procedures and local blocks, if within extent and ability, can spare systemic medicine exposure.
For clients with material use problems, assume a higher standard tolerance and a higher danger of breathing clinical depression if sedatives or alcohol are on board. Offer analgesia without judgment, yet plan for airway support. Involving allied health and wellness early, when feasible, improves longer-term outcomes and lowers the rotating door effect.
When the medical diagnosis hides under the pain
Not every unpleasant discussion is a thumbs-up for overview of pain management course full-dose opioids. Severe abdominal areas with unclear etiology, severe headache with neurologic changes, or breast discomfort with hemodynamic instability each calls for a deliberate speed. The old myth that analgesia obscures diagnosis has actually been greatly debunked, yet timing and choice of representative still matter.
For thought stomach catastrophes, moderate, titrated analgesia combined with careful review protects test energy while appreciating the client's distress. In severe headache with warnings, deal with discomfort while moving swiftly toward definitive imaging and helpful care, defending against oversedation that may shadow neurologic assessments. Chest discomfort requires synchronized analgesia and antiplatelet or anticoagulant treatment per protocol, alongside rhythm surveillance and nitrates if shown. Good care lives in assimilation, out single-track thinking.
Training that changes just how you practice
The finest discomfort monitoring programs develop muscle mass memory under sensible restrictions. Manikins and case situations are useful, yet nothing replaces live, messy practice: choosing application while the blood pressure alarm tweets, coaching breathing through contractions while a 2nd client calls your name, or evaluating the risks of one more fentanyl aliquot in a client whose oxygen saturation just dipped.
When choosing a pain management certification course, look for programs that incorporate:
- Scenario-based simulations that call for prioritization, reassessment, and handover under time pressure Pharmacology sessions that teach device, communications, and damaging occasion management, not simply dosing tables
Assessment must be greater than a created examination. Expertise demonstrations, medication preparation drills, damaging event recognition, and interaction circumstances disclose whether learning translates to action. For nurses branching right into urgent care or retrieval settings, pain administration courses for nurses that incorporate PUAEME008 expertises with triage systems and neighborhood formularies offer the most effective worth. Physiotherapists working in severe musculoskeletal settings likewise benefit from discomfort monitoring programs for physiotherapists that highlight nonpharmacologic strategies together with interdisciplinary sychronisation; if pharmacologic administration is out of scope, the training should still cover recognition of undertreatment and rise pathways.
Short training courses in pain administration can be beneficial, but examine that "short" does not imply shallow. A focused one-day program can supply targeted skills, for example, intranasal analgesia in pediatric medicines or ketamine titration for injury, provided it consists of supervised method and post-course pain management certificate course mentoring. A certification course in pain monitoring that assures broad capacity ought to include monitored professional time or durable simulation to warrant a discomfort management certification.
Documentation safeguards people and clinicians
No one takes pleasure in paperwork in the warmth of method, yet a clean document becomes part of the treatment. It tells the following clinician what functioned and what did not, it secures the person from duplicated dosing, and it shields you when results are examined days later.
Elements to tape include the baseline discomfort description, objective indications, the rationale for agent selection, dose and time, path, patient reaction, vitals fads, damaging occasions and mitigation, and the web content of the handover. If you deviated from a basic series as a result of a patient-specific variable, compose the factor in a full sentence. That behavior develops trust in your scientific judgment.
Building a society of prompt analgesia
Individuals can exercise well, yet systems still fail people if society punishes analgesia as risky or optional. I have operated in services where pain relief needed 3 trademarks, and the foreseeable result was experiencing. It took a data-driven debate to transform minds: time to initial analgesia stopped by 40 percent after protocol simplification, and there was no rise in respiratory system compromise when keeping an eye on standards were maintained. The leadership after that embedded analgesia metrics into high quality dashboards, and the culture shifted.
If you remain in a position to affect plan, advocate for very easy access to accepted representatives, standardized checklists for prep work and tracking, and routine case evaluates that concentrate on finding out instead of blame. Connection pain metrics to person experience comments, not as a score to chase thoughtlessly, but as one crucial indicator of compassionate care.
Practical ideas from the field
Over years of training PUAEME008 give discomfort management, a couple of small habits keep paying off.
- Prime your kit for the initial 10 minutes. Maintain intranasal atomizers preloaded and classified by dose variety, methoxyflurane available, and tape pre-cut for splints. The faster you can act, the cleaner your decision-making.
Practice a dose-talk script. Clients and households unwind when they listen to positive, consistent explanations: call the medicine, anticipated advantages, usual adverse effects, and what you will certainly do to monitor.

Think in sets. One clinician prepares and administers, the other watches respiratory tract, air flow, and psychological condition. Even in a tiny group, assign roles clearly for risky moments.
Use the discomfort scale as a discussion starter, not a verdict. Ask what number would certainly let them move or breathe even more conveniently, after that go for that target instead of zero.
Plan the next step before you supply the current one. If this dose does not work, what is your 2nd line, what are the contraindications, and when will certainly you reassess?
Those micro-skills make the distinction between positive treatment and chaotic improvisation.
Where PUAEME008 fits among more comprehensive certifications
Many clinicians collect badges, and not all badges convert to much better treatment. A pain administration certification proves you have satisfied a requirement, yet recurring capability comes from calculated technique. If you are thinking about a discomfort administration qualification course, align it with your work environment. Prehospital medical professionals benefit from programs connected to real operational drug listings, gadgets, and documentation systems. Hospital-based team might prefer modules that cover nerve blocks, mixture pumps, and multimodal analgesia pathways.
For nurses in immediate treatment or ED triage functions, discomfort administration training for nurses that blends pharmacology, trauma evaluation, and interaction training boosts both throughput and person fulfillment. For allied health experts, a pain administration certificate course can clear up borders and acceleration paths, stopping unsafe hold-ups when pharmacologic pain control is appropriate.
The highest-yield programs close the loophole with mentorship. A single day of talks does not alter reflexes. A month of on-shift coaching does.
Measuring success beyond the discomfort score
Pain ratings relocate the needle, but they are not the only result worth tracking. I seek fewer unscheduled returns due to inadequate analgesia, much shorter time to mobilization in basic fractures, lower incidence of oxygen desaturation throughout opioid use, and much better handover quality. Individual comments tell you more than survey numerics. If clients state feeling listened to, safe, and sustained, your analgesia practice is most likely sound.
Systems that installed PUAEME008 standards see downstream gains in sedation security, reduced frustration during transport, and tighter team effort. Those gains compound. Less disorder suggests less errors, and fewer mistakes mean even more power for the following person that requires your ideal judgment.
Final ideas from the sharp end
Pain is a scientific problem and an ethical one. When someone trusts you with their suffering, they are not asking for heroics. They are requesting for attention, ability, and follow-through. PUAEME008 orders that agreement into proficiencies you can practice, test, and refine.
If you are picking amongst pain management training programs, select the one that requires your existence, not simply your attendance. Ask exactly how they teach emergency discomfort administration under sensible restraints, exactly how they examine communication, and how they keep your skills alive after the certification is mounted. Whether you are exploring a give pain management course as your very first step or including a discomfort administration certification to an established occupation, deal with the system as the beginning of a behavior: examine with curiosity, treat with precision, and circle back to see if you truly helped.
The days that stick with me are not the huge saves. They are the silent wins, like the anxious youngster who was laughing by the time we reached radiology since someone took five extra minutes to describe the intranasal spray and hold a hand. That is the basic worth training for, and the pledge behind any kind of program that declares to educate pain well.